What is Medical Billing?
Medical billing is the process of generating, submitting, and following up on claims with insurance payers (government and commercial) to receive payment for medical services rendered by healthcare providers. It acts as a financial bridge between patients, healthcare providers, and insurance payers. Accurate medical billing ensures that medical services are properly documented and translated into standardized codes for correct payment processing.
In this process, medical billers utilize standardized coding systems, such as ICD-10, CPT, and HCPCS, which are essential for translating procedures, diagnoses, and medical services into universally recognized codes. This ensures accurate claim preparation, which becomes ready to be reimbursed. After submitting a claim, medical billers follow up with insurance payers to ensure the provider receives appropriate reimbursement for their services.

What is the Medical Billing Process?
The medical billing process is a structured workflow that converts patient care into financial reimbursement. It involves multiple coordinated steps that ensure healthcare providers receive accurate and timely payments for their services. Each step plays a crucial role in maintaining compliance and revenue consistency.
-
Patient Registration
The medical billing process begins when a patient books an appointment with a provider. Medical billers collect and document accurate patient information, including medical history, insurance details, and other relevant data for registration purposes. Even the slightest inaccuracies result in claim denial for the providers.
-
Insurance Verification
After patient registration, insurance verification specialists confirm the patients’ eligibility and coverage. Some procedures also require pre-authorization from the insurers before the services are rendered.
-
Medical Coding
Once the patients’ insurance coverage is verified and after obtaining all the required authorizations, the next step is medical coding. The medical coding process is the translation of clinical notes into standardized codes such as CPT, ICD-10, and HCPCS. Accurate coding ensures proper claim preparation and correct reimbursement.
-
Creating Superbill
Once the patient’s visit is completed and they’ve walked out, the next step is to create a superbill. A superbill is a foundational document for reimbursement claims that contains all the necessary information about the provider, the patient, and the visit, ensuring that the claim is complete and accurate for smooth processing.
-
Claim Submission
After reviewing the superbill and attaching all the supporting information, medical billers convert that data into an official insurance claim. While the superbill is an internal document used within the healthcare facility, a medical claim is a formal request generated for the insurance companies. Any incorrect or mismatched information in this stage leads to claim rejection — that is why accuracy is crucial for successful reimbursement.
-
Payment Adjudication & Monitoring
Once the claim is submitted, insurance companies review and process it through a process called payment adjudication. After the review, the insurer sends payment postings to providers that contain all the details — including the amount paid or adjusted, and whether the claim was approved or denied.
Medical billers carefully administer the adjudication process to ensure the payments are accurate and aligned with the billed services. This helps maintain a proper reimbursement flow.
-
Issuing Patient Statements
After the insurance adjustments and payments, the remaining balance becomes the patient’s responsibility. Patient statements provide a detailed overview of every payment received, along with the outstanding amount. This ensures transparency and helps the patients understand their financial obligations.
Medical billers also follow up with the patients to ensure smooth revenue collection for the provider.
-
A/R Follow-Up
A/R follow-up is the process of tracking and collecting payments owed by insurance companies and patients. It is the most crucial step to ensure all balances are collected timely. It also double-checks claims to identify if a claim was lost or delayed in the process.
The provider’s team contacts payers and resolves errors to recover lost revenue. Effective A/R management helps maintain a healthy cash flow by ensuring accurate payments for services rendered.

Why is Medical Billing Important in U.S Healthcare?
Medical billing is essential to run the entire US healthcare system smoothly. It includes everything from managing finances to supporting patient care. Accurate medical billing keeps healthcare providers’ practice revenue reliable, consistent, and smooth.
-
Organize Healthcare Revenue
- Track charges
- File claims
- Manage incoming payments
-
Ensure Timely Reimbursements
-
Support Sustainable Care
- Better staff
- New equipment
- Reliable patient services
- High-quality care
- Long-term growth
-
Reduce Administrative Burden
-
Improve Billing Accuracy
-
Enhance Patient Transparency
Medical billing ensures financial health and sustainability in medical practices. It helps the providers get properly paid for their services. The medical billing system creates and organizes a structured process to:
Medical billing ensures quick and accurate claim submissions. Medical billers ensure timely submissions and proper follow-up to help get faster reimbursements. Timely claims prevent denials and delays and also reduce the wait time for payments.
Accurate billing increases the financial stability of a practice. Timely reimbursements mean the providers are able to invest in:
Medical billing requires a lot of paperwork handling in claim processing. Medical billing professionals free up healthcare providers from administrative burden. This helps the providers focus more on patient care. Outsourcing the billing process reduces stress and time spent on paperwork tasks.
Skilled billing professionals perform accurate claim processing, which improves billing accuracy. Incorrect billing results in claim denials or delayed payments. Therefore, medical billing experts ensure smoother claim approvals for a better patient experience.
A transparent medical billing process helps the patient understand finances better. It reduces confusion and helps them make informed decisions about their treatment plans. Medical billing turns a complex financial process into a simplified and transparent workflow.

What are the Main Types of Medical Billing?
Medical billing can be categorized based on the claim-based approaches, which include professional billing and institutional billing.
-
Professional Billing
-
Institutional Billing
-
Front-End Billing
-
Back-End Billing
Professional billing refers to the medical claims that are submitted for services provided by individual healthcare professionals. It includes doctors, nurses, and therapists. They mainly provide healthcare services in outpatient clinics and private practices.
The claim form used for professional billing is CMS-1500.
Institutional billing is used for the services rendered in an institution. Such institutions include hospitals, rehabilitation centers, and large healthcare facilities. It includes the charges for institutional facilities as well, such as room fees, equipment use, and nursing fees.
Medical billers use UB-04, also known as the CMS-1450 form, for institutional billing.
To represent the different stages of the medical billing workflow, it can also be categorized into process-based approaches. It includes front-end billing and back-end billing.
All the medical activities that occur before a claim is submitted are covered by front-end billing. These activities include patient registration, pre-authorization, insurance verification, and charge capture. Accurate front-end billing ensures a smooth claim submission process while also preventing claim denials.
Back-end billing covers all the medical services that start after a claim is submitted. These services include patient statement, claim follow-up, payment posting, A/R follow up and denial management. It ensures accurate and timely reimbursements for the services rendered.

What Tools and Softwares are used in medical billing?
From patient scheduling to reimbursements, medical billing requires a wide range of digital tools to reduce the chances of errors. It is essential to streamline operations and ensure accurate reimbursements. Such tools improve efficiency while allowing a better communication channel between providers, patients, and the insurers. It also helps the practices stay compliant with payer-specific rules and HIPAA guidelines.
The following are a few of the many tools and software used in the medical billing industry:
-
Kareo
A user-friendly platform with patient engagement tools. It is commonly used by small practices in the USA.
-
Athenahealth
It is a cloud-based software that is known for its practice management features.
-
AdvancedMD
AdvancedMD offers patient portals and provides telehealth services to its clients. It also offers comprehensive tools for revenue cycle management.
-
EHR Integrations / API Tools
EHR integration is a great way to sync clinical documentation with billing workflows. This ensures accurate billing and coding while keeping everyone updated.
-
Practice Management Systems Software
Practice management systems are crucial to handle the billing process from scheduling to financial reporting.
-
Clearinghouse Platforms
These platforms scrub claims to identify errors and submit them accurately to insurance companies. They act as an intermediary between the provider and the insurer.
-
Coding Software Tools
Coding software tools help the billers assign accurate ICD, CPT, and HCPCS codes. They also verify coding rules to avoid errors resulting in claim denials.
-
Coding and Compliance Tools
Such tools help the medical billers in assigning the correct ICD, CPT, and HCPCS codes. It also helps them stay compliant with the payer rules. Some of the examples of coding and compliance tools are TruCode Encoder, 3M CodeFinder, and Codify by AAPC.
-
Payment Processing Software
Payment processing systems streamline the money movement between patients, insurers, and providers. This minimizes errors and improves cash flow while securely handling the confidential data. It includes:
- Co-Pay collection
- Patient balance management
- Security and Compliance

Ethical Considerations in Medical Billing
Ethical considerations in medical billing are the key to maintaining accuracy, transparency, and compliance. They ensure that all financial transactions between patients, providers, and insurers are handled responsibly and fairly. It also helps maintain trust and financial integrity throughout the entire reimbursement process. The role of ethical considerations is to maintain a balanced system that promotes accuracy, fairness, and compliance. Some of the key ethical principles include:
-
Fair Billing Practices
One of the most important ethical aspects of medical billing is to charge only for services that have been actually provided. Practices such as upcoding, unbundling, or charging for non-rendered services are strictly unethical and can lead to legal penalties and loss of patient trust.
-
Handling Errors
It is essential to identify and correct mistakes in coding and billing promptly. Open communication and transparency are key to minimizing errors and maintaining trust with both patients and insurers. A responsible biller always reviews and verifies claims before submission.
-
Confidentiality and Data Security
According to HIPAA regulations, billing professionals are required to safeguard all sensitive patient data. Both financial and health-related information must remain private and protected through secure data handling practices and authorized access controls.
-
Timeliness in Billing and Payments
It is an ethical duty for medical billers to submit and process payments within an appropriate timeframe. Delays in billing disrupt a provider’s cash flow and create operational inefficiencies. Ethical billing professionals ensure timely claim submissions and prompt denial management to maintain steady reimbursements.
-
Transparency in Third-Party Partnerships
Healthcare providers relying on clearinghouses or external billing companies must disclose these partnerships responsibly. Patients should be informed if third-party services have access to their billing or health data. Transparent communication builds patient confidence and upholds ethical standards in healthcare administration.

Compliance Standards in Medical Billing
Compliance standards are set to ensure that all billing activities follow federal and state regulations and payer policies. These standards protect patients, providers, and the insurers from financial mismanagement. It also promotes a transparent medical billing reimbursement process.
Some of the most important regulations of medical billing compliance are:
-
Federal and State Laws
Medical billers need to stay updated on policy and compliance changes, as each state regularly revises its own regulations and requirements.
-
Health Insurance Portability and Accountability Act (HIPAA)
HIPAA ensures confidentiality and patient privacy related to health and financial information.
-
Centers for Medicare and Medicaid Services (CMS)
CMS issues rules for billing, coding, and claim submission under Medicare and Medicaid programs. Non-compliance leads to claim denials and audits.
-
False Claims Act (FCA)
FCA prohibits the submission of false claims, like upcoding, duplicate billing, and unrendered services.
-
Stark Law (Physician Self-Referral Law)
The Stark Law restricts physicians from referring patients to facilities in which the doctors or their family members have a financial interest.
-
OIG Compliance Program Guidelines
The Office of Inspector General (OIG) encourages regular audits and training. This helps prevent errors before they lead to violations.
-
Anti-Kickback Statute (AKS)
To promote fair and unbiased patient care, the AKS prohibits financial incentives and referrals that could influence healthcare decisions.

What are the Challenges in Medical Billing?
Medical billing comes with its own set of challenges that can affect a healthcare provider’s revenue cycle, efficiency, and compliance. Understanding these issues helps organizations create effective strategies for better financial management and patient satisfaction.
-
Claim Denials and Rejections
Claim denials are known to slow down the cash flow of a practice. Denials can occur because of several issues, such as incorrect patient demographics, eligibility issues, or missing pre-authorizations.
-
Delayed Payments
Timely follow-up, transparency, and clear patient communication are the keys to maintaining a steady revenue cycle. Payments are often delayed because of payer backlogs and patient non-payment.
-
Constantly Changing Regulations
Healthcare laws and insurance policies constantly change with frequent updates. Failure to comply with these regulations results in claim denials and legal penalties.
-
Coding Errors
Incorrect coding is one of the main causes of claim denials. Undercoding, upcoding, and missing modifiers trigger compliance issues and delay reimbursement.
-
Staff Training
Frequent policy updates and coding revisions require continuous learning. Ongoing staff training is crucial for maintaining compliance, accuracy, and efficiency.
-
Data Breaches
Digital medical billing processes increase the risk of data breaches. Medical billing systems must protect sensitive patient information under HIPAA regulations. It is essential to implement data encryption and robust cybersecurity protocols to overcome these challenges.
-
Coordination Between Providers, Insurers, and Medical Billers
Proper communication between all the parties leads to efficient billing. Incomplete information from providers results in billing errors and missed deadlines. However, the use of practice management systems creates a streamlined workflow, which helps in reducing these challenges.
-
Maintaining Patient Confidentiality
Maintaining patient confidentiality is a growing challenge with the increasing use of digital platforms. Medical billers need to follow HIPAA compliance standards to keep sensitive health and financial information secure.

How are Technology and AI transforming Medical Billing?
The technology and AI have made the medical billing process a more automated, efficient, and accurate method. Automation tools such as RPA (Robotic Process Automation) are replacing repetitive and time-consuming tasks to minimize denials caused by missing or incorrect information.
AI-powered coding has revolutionized the medical coding process. Natural Language Processing (NLP) is now interpreting clinical notes to speed up claim creation. AI-assisted coding tools learn from previous claim data and recommend the most optimized and compliant coding practices.
Apart from that, advanced algorithms automatically monitor billing activities to help detect potential compliance violations. Predictive denial management uses AI to detect duplicate billing and upcoding before they become a serious issue. This ensures that billing stays in line with the HIPAA, CMS, and OIG guidelines.

What is the Difference Between Medical Billing and Coding?
| Medical Billing | Medical Coding |
|---|---|
| Medical billing is the process of managing, preparing, and submitting insurance claims for the services rendered by patients. | Medical coding is the process of translating medical reports, procedures, and diagnoses into standardized alphanumeric codes. |
| The purpose of medical billing is to ensure that healthcare providers receive timely and accurate payments. | Medical coding’s purpose is to ensure accurate representation of all the services and patient care for compliance. |
| The tools used for medical billing are clearinghouses, payer portals, billing software, and accounting systems. | Medical coding requires tools like ICD-10, CPT, HCPCS manuals, and EHR systems. |

What Are the Key Terms in Medical Billing?
Understanding common terms in medical billing helps providers, billers, and patients navigate the complex reimbursement system efficiently. Below are some key terms every billing professional should know:
-
Claim
A claim is a formal request submitted by healthcare providers to insurance companies for payment of services rendered to patients. It contains all the details regarding treatment and charges. The insurance company reviews the claim and reimburses according to the patient’s coverage.
-
Deductible
A deductible is the amount of money that a patient must pay annually before their insurance coverage begins. Once this amount is paid, the insurance company starts covering the remaining eligible medical services.
-
Electronic Data Interchange (EDI)
EDI is the electronic transmission of healthcare data between providers and insurers. It is a secure digital network that speeds up the process and reduces paperwork, replacing traditional manual systems.
-
Electronic Funds Transfer (EFT)
EFT is a secure digital method of transferring funds directly from the insurance company to the healthcare provider. This ensures faster reimbursements, greater accuracy, and replaces paper-based check payments.
-
Electronic Remittance Advice (ERA)
ERA is a digital document sent by insurance companies that outlines the details of claim processing, including:
- Billed amount
- Allowed amount
- Deductibles
- Payments made
- Patient responsibility
- Reason codes
ERA helps healthcare providers and medical billers understand post-payment details and reconcile accounts more accurately.
-
Co-pay
A co-pay is a fixed amount a patient must pay at the time of service. After that, the insurance company covers the remaining cost. Co-pays vary depending on the service type and insurance plan.
-
Coinsurance
Coinsurance is a cost-sharing arrangement where patients and insurers split the cost of medical expenses after the deductible has been met — typically expressed as a percentage.
-
Adjudication
Adjudication is the process by which an insurance company reviews, approves, or denies a medical claim based on the policy terms, coverage limits, and medical necessity of the treatment.
-
Global Period
The global period is a timeframe set by insurance companies during which all routine care related to a procedure is covered under a single payment. It simplifies billing and prevents duplicate charges for the same treatment.
-
Medicare Administrative Contractor (MAC)
MACs are private organizations hired by Medicare to process claims and handle appeals. Each MAC operates within a designated geographic region to ensure compliance and efficiency.
-
Medicare Beneficiary Identifier (MBI)
MBI is a unique, randomly generated number assigned to Medicare beneficiaries. Its primary purpose is to protect patient identities and ensure secure claim processing.
-
Clearinghouse
Clearinghouses act as intermediaries between healthcare providers and insurance companies. They review claims for errors, ensure compliance with payer-specific requirements, and streamline submissions to enable faster claim approvals.

What are Medical Billing Codes?
Medical billing codes are standardized codes that the healthcare providers use to describe services, procedures and diagnoses. These codes ensure that the healthcare documentation is translated in a universal language for accurate claim submissions and reimbursements. Medical billing codes also help maintain compliance with the federal and insurance regulations. Some of the most common medical billing codes are:
A. CPT Codes
Healthcare providers use Current Procedural Terminology codes to describe surgical and diagnostic services in professional billing. The American Medical Association has set and condensed these codes into five digits. They inform the payers about:
- Office visits
- Minor surgeries
- Injections
B. HCPCS Codes
Healthcare Common Procedure Coding System Level II codes highlight medical equipment and certain medications. These codes are essential for the professional billing of Medicaid and Medicare. They cover:
- Prosthetics
- Ambulance rides
- Durable medical equipment (DME)
- Medications
C. ICD-10 Codes
International Classification of Diseases codes explain a patient’s diagnosis. They provide a reason for the services provided to patients. Each code represents the medical condition or symptom necessary for the insurance approval.
What is a Revenue Code in Medical Billing?
A revenue code refers to the three or four-digit code used in healthcare facilities to represent the type and location of the services provided to the patients. It helps the insurance companies identify the kind of care, department, and category of service being billed. The revenue code helps ensure accurate payment, along with classifying costs for reimbursement. It also helps prevent claim denials by matching the services with the right CPT/HCPCS codes.
What is MSP Code in Medical Billing?
MSP in medical billing stands for Medicare Secondary Payer code. It states the reason for Medicare being the secondary payer for a patient’s medical claim. MSP code indicates the specific situation that determines which insurance company is responsible for paying before Medicare. MSP code also helps prevent duplicate payments by Medicare.
What is an Entity Code in Medical Billing?
An entity code in medical billing helps identify each participant and their role in a medical claim. Such participants include billing provider, referring provider, policyholder, and the insurance company. It helps ensure that each claim is routed and processed accurately.
What is Entity Code Rejection in Medical Billing?
An entity code rejection in medical billing occurs when the claim is rejected because of an unidentified entity. It means that the information of that person or organization is either missing, incorrect or improperly identified.

Who Performs Medical Billing?
Medical Billing is a collaborative process handled by multiple specialists. Each professional plays a vital role in properly documenting, coding, and submitting claims. This results in maximum reimbursements for the practice.
Medical Billing Specialists
- Reviewing clinical documentation
- Preparing accurate insurance claims
- Entering patient demographics and insurance information
- Ensuring the claims are complete and compliant
- Submitting claims electronically through payer-specific portals
- Running the claims from clearinghouses for double-check
- Tracking claims through the adjudication process
- Posting payments received from insurance companies
- Handling claim denials
- Resubmitting corrected claims for reimbursement
- Filing an appeal if necessary
Front Office Staff
Front office staff play a crucial part in reducing the administrative burden on the providers. Any minor error of misspelling or incorrect data leads to denial. Their role includes:
- Registering new patients
- Verifying insurance information
- Inputting credentials into the system
- Collecting co-pays or deductibles from the patients
- Scheduling follow-up appointments
- Outsourced billing companies
Most of the providers prefer to outsource their billing to third-party companies. They provide end-to-end billing services from appointment scheduling to payment being received. These remote companies save the providers from overhead costs. Billing companies are proficient in using advanced software for performance tracking. They hold in-depth knowledge in every specialty and tailor their services accordingly.
Medical Coders
Medical coders have special training in translating clinical notes into diagnostic and procedural codes. Their role includes:
- Reviewing clinical charts
- Cross-checking documentation
- Assigning accurate codes to diagnosis or treatment procedures
- Ensuring the medical necessity of medical services
- Following coding guidelines
Revenue Cycle Managers
Revenue cycle managers overlook the entire process to ensure smooth revenue flow. Their role includes:
- Setting billing and collection policies
- Monitoring A/R
- Identifying inefficiencies
- Driving improvements for better cash flow
- Keeping billing teams, providers, and patients in the loop
- Providing staff with regular training on compliance
- Optimizing the overall financial performance
Insurance Verification Specialists
Insurance verification specialists come in before the patient walks into the clinic. Their role is:
- Ensuring the patient’s insurance is active
- Confirming the procedure’s coverage in the patient’s plan
- Checking if the service requires pre-authorization
- Identifying limitations and exclusions
- Clarifying the patient’s out-of-pocket costs
- Helping to prevent claim denials by ensuring accurate insurance details
Accounts Receivable Specialists
A/R specialists are the key to increasing collection rates and maintaining healthy cash flow for the provider’s practice. Their role includes:
- Monitoring outstanding claims
- Following up with insurers and patients
- Handling appeals
- Reviewing secondary claim submissions
- Resolving payment delays
- Posting technical and reimbursement issues
Compliance Officers
Compliance officers protect the providers from audits, penalties, and loss of reputation. Their role is:
- Monitoring HIPAA compliance adherence
- Reviewing coding guidelines
- Conducting internal audits
- Reviewing clinical charts
- Training staff on ethics
- Responding to legal issues

Medical Billing Services
Medical billing services are the backbone of healthcare revenue management. It connects patient care with financial stability by ensuring accurate reimbursements. The medical billing services start from when a patient books their appointment. It continues until the payment of the accurate outstanding balance. It also helps ensure that every service provided to the patients is billed, coded and reimbursed according to the federal guidelines and payer policies.
When Should You Consider Outsourcing Medical Billing?
Medical billing outsourcing refers to the process of giving a healthcare provider’s billing and claims management tasks to an external company, specialized in this domain. Healthcare providers are recommended to consider outsourcing their medical billing. It helps improve accuracy and precision in claim processing. Outsourcing medical billing services is more than just paperwork. It requires detailed knowledge of coding systems, payer guidelines, and compliance regulations. The medical health professionals start to outsource their medical billing services if they face problems with the following issues:
- Staff Overload: Sometimes, the practice’s staff gets overwhelmed with the administrative burden of medical billing. This causes delays in claims submissions and follow-ups.
- High Error Rate: Outsourcing becomes important when billing errors and claim denials increase. They can slow down operations and reduce the practice’s income.
- Poor Cash Flow: Inaccurate billing often results in poor cash flow. This becomes a hurdle for many day-to-day practice operations. It includes investing in new equipment and paying the staff. Outsourcing helps provide a steady cash flow.
- Lack of Expertise: Outsourcing is important for handling complex specialties and implementing payer-specific rules. Front-desk staff often lack this expertise, resulting in claim denials and slow reimbursements.
Why Outsource Medical Billing Services?
Outsourcing medical billing services is essential for the healthcare providers so they can focus more on patient care. The trained billing professionals handle all the complex financial and administrative tasks to reduce errors and improve billing efficiency. The medical billers also ensure compliance while saving the operational costs of a practice.
What are the Benefits of Outsourcing Medical Billing Services?
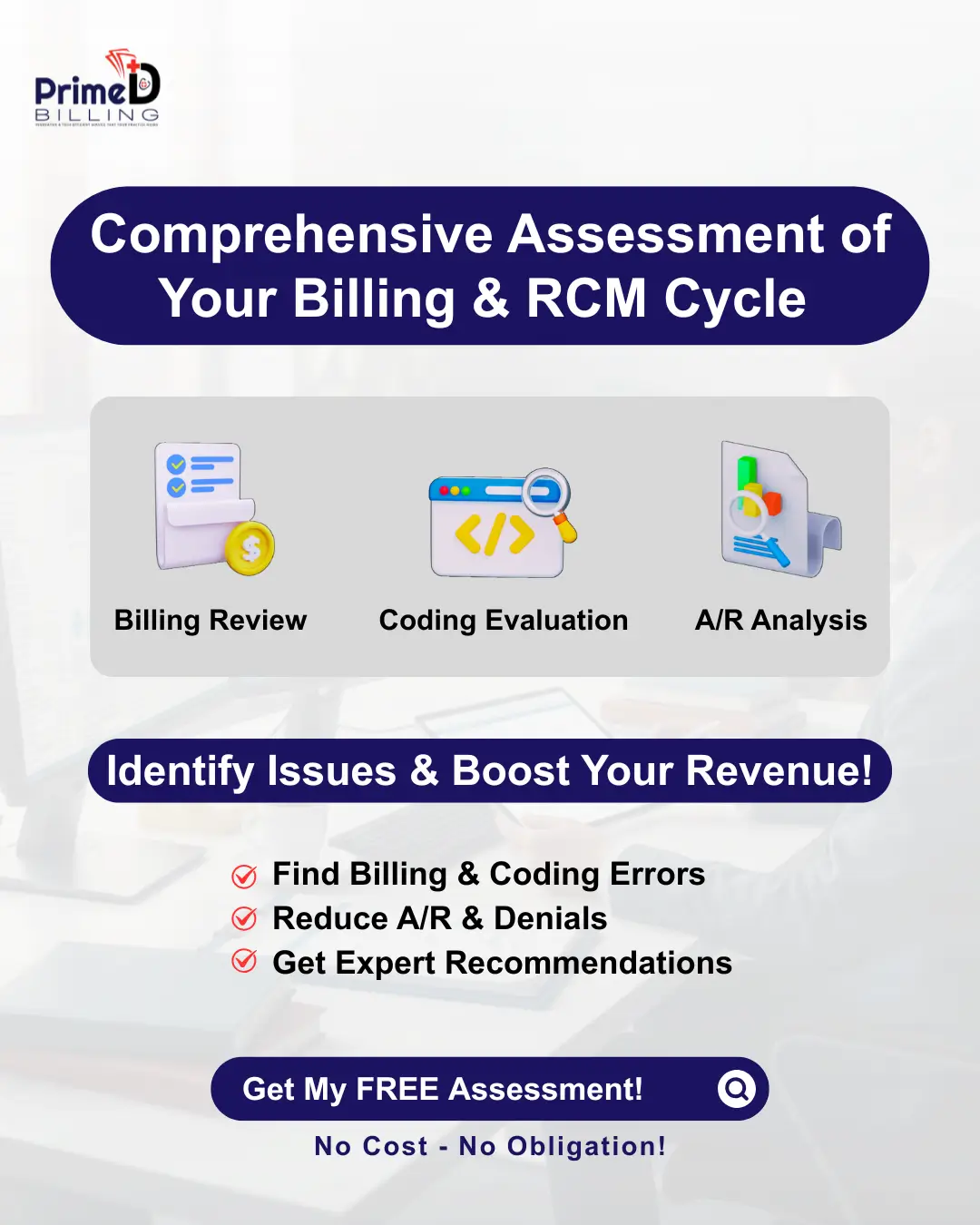
Efficient medical billing is a must in today’s fast-paced healthcare environment. From claim submissions to timely reimbursements, the process ensures compliance while also maintaining accuracy. Outsourcing medical billing improves cash flow for the practice. This contributes to enhancing revenue cycle efficiency.
Revenue cycle efficiency refers to improving the accuracy of the existing revenue cycle. This ensures faster reimbursements. It begins with proper charge capture. Outsourcing medical billing is necessary for the financial health of a medical practice.
Medical billing companies have dedicated teams. These teams proactively follow up on unpaid claims. This helps the money stay in the practice. They also ensure consistent collections to stabilize the cash flow. A dedicated medical billing team helps process clean claim submissions, follow-ups, denials, and appeals. It helps the medical staff improve overall patient experience while also reducing burnout.
Outsourcing medical billing lowers the operational cost of a practice. It includes eliminating hidden costs along with salaries, training, and compliance updates. It also helps save the need for extra office space and equipment.

In-house vs Outsourced Medical Billing
In-house billing refers to when the healthcare provider’s own staff handles all the billing internally. The healthcare providers have direct control over billing operations. However, it requires high set up costs, including training, salaries, and software. Along with that, in-house medical billing faces a higher risk of human errors or delays.
Outsourcing, on the other hand, refers to when an external company who specializes in medical billing and revenue cycle management handles the provider’s medical billing services. Healthcare providers rely on a third party for professional expertise on medical billing services when they consider outsourcing. It requires a relatively low setup cost for service fees only.

How to Choose a Medical Billing Partner for Outsourcing?
It is essential to focus on factors that deeply impact the revenue cycle of a practice before choosing a medical billing partner for outsourcing. A reliable partner must have robust security protocols and up-to-date knowledge of payer-specific rules. Commitment to compliance is the basic component to look for in a medical billing partner.
Another key factor in selecting a medical billing company is experience. It helps them manage claim submission and denial resolutions on an advanced level. Along with that, a partner with better technology for advanced billing software, real-time reporting tools, and automated claim scrubbing enhances the practices’ accuracy and efficiency.
Transparent pricing models of a medical billing company also play an important role in aligning the fees with measurable outcomes. Such outcomes include faster collections and reduced denials.
Lastly, effective communication is the key to transparency and accountability. Choosing a partner that offers regular performance reports and addresses queries promptly can truly streamline the practice’s revenue cycle, supporting it in long-term success.
Partner with Prime Doc Billing Today
Let our experts handle your billing — streamline your revenue cycle and focus on patient care.


 (347) 650-2656
(347) 650-2656



 info@primedocbilling.com
info@primedocbilling.com